Ultrasound images Portal hypertension
Portal hypertension occurs when the pressure in the portal venous system is raised. This may happen as a result of chronic liver disease, particularly in the cirrhotic stage, when the nodular and fibrosed nature of the parenchyma impedes the flow of blood into the liver. It is significant because it causes numerous deleterious effects on the patient, many of which can be recognized on ultrasound (Table BELOW).

Raised portal venous pressure is associated with several complications: Portal vein signs Portal vein (PV) flow is influenced by numerous factors, including prandial state, patient position, exercise and cardiac output. Its velocity varies considerably in both cirrhotic and healthy subjects, and it is essential to use colour and spectral Doppler to investigate the portal flow
● normal in direction (hepatopetal) and velocity.
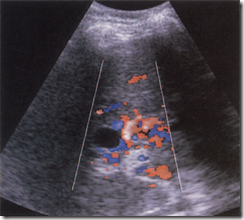
● reduced in velocity (Fig. A), < 10 cm/sec, although there is overlap with the normal range.
● damped, in which there is a lack of normal respiratory variation of both the calibre and the waveform of the splenic and portal veins. The normal spectrum has a ‘wavy’ characteristic, which may be lost.
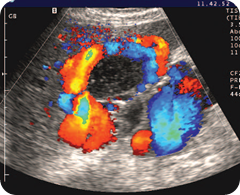
● reversed (hepatofugal) (Fig. B). This indicates serious liver disease. Interestingly, patients with hepatofugal PV flow are much less likely to suffer from bleeding varices, suggesting a type of ‘protective’ mechanism here.
● balanced, in which both forward and reverse low velocity flow is present, a condition which may precede imminent thrombosis (Fig. C).
● thrombosed (Fig. D). Low-level echoes from the thrombus may be evident but with fresh thrombus the vein may appear anechoic, as in the normal vein. Although PV thrombosis most commonly results from portal hypertension in cirrhosis, there are many
● reduced in velocity (Fig. A), < 10 cm/sec, although there is overlap with the normal range.
● damped, in which there is a lack of normal respiratory variation of both the calibre and the waveform of the splenic and portal veins. The normal spectrum has a ‘wavy’ characteristic, which may be lost.
● reversed (hepatofugal) (Fig. B). This indicates serious liver disease. Interestingly, patients with hepatofugal PV flow are much less likely to suffer from bleeding varices, suggesting a type of ‘protective’ mechanism here.
● balanced, in which both forward and reverse low velocity flow is present, a condition which may precede imminent thrombosis (Fig. C).
● thrombosed (Fig. D). Low-level echoes from the thrombus may be evident but with fresh thrombus the vein may appear anechoic, as in the normal vein. Although PV thrombosis most commonly results from portal hypertension in cirrhosis, there are many
FIG. A
Ultrasound images Portal vein (PV) velocity is greatly reduced
FIG. B Ultrasound images Reversed PV flow in portal hypertension. Note the increased velocity of hepatic arterial flow indicated by the light colour of red just anterior to the portal vein. The patient has macronodular cirrhosis with ascites.
fig C
ultrasound images Balanced PV flow. Alternate forward and reverse low-velocity flow on the Doppler spectrum. The PV colour Doppler alternates red and blue
Fig. D
Ultrasound images PV thrombosis. The PV is dilated (arrows) and filled with thrombus. A collateral vessel is seen anterior to this—not to be confused with the PV—as this is a source of false-negative ultrasound results
Fig. E
Ultrasound images Non-dilated, thrombosed PV (arrow) with collaterals demonstrated on power Doppler.
other causes, including inflammatory or malignant conditions which may surround, compress or invade the portal and/or splenic veins The thrombosis may be total or partial.
● hepatopetal main PV flow with hepatofugal peripheral flow may be a sign of HCC, requiring careful scanning to identify the lesion.
● cavernous transformation. A network of collateral vessels may form around a thrombosed main portal vein at the porta, especially if the thrombosis is due to extrahepatic causes (for example pancreatitis) rather than diseased liver. The appearance of cavernous transformation of the PV is quite striking (Fig. A 1) and colour Doppler is particularly useful in its diagnosis. Make sure, before diagnosing PV thrombosis, that the vein axis is less than 60° to the transducer and that the Doppler sensitivity is set to pick up lowvelocity flow. Ultrasound is known to have a falsepositive rate for PV thrombosis but this is often due to inadequate technique or insensitive equipment. False-negative results, indicating that flow is present in a vein which is actually thrombosed, are due to the detection of flow within a collateral vessel at the porta, which can be mistaken for the main PV
● hepatopetal main PV flow with hepatofugal peripheral flow may be a sign of HCC, requiring careful scanning to identify the lesion.
● cavernous transformation. A network of collateral vessels may form around a thrombosed main portal vein at the porta, especially if the thrombosis is due to extrahepatic causes (for example pancreatitis) rather than diseased liver. The appearance of cavernous transformation of the PV is quite striking (Fig. A 1) and colour Doppler is particularly useful in its diagnosis. Make sure, before diagnosing PV thrombosis, that the vein axis is less than 60° to the transducer and that the Doppler sensitivity is set to pick up lowvelocity flow. Ultrasound is known to have a falsepositive rate for PV thrombosis but this is often due to inadequate technique or insensitive equipment. False-negative results, indicating that flow is present in a vein which is actually thrombosed, are due to the detection of flow within a collateral vessel at the porta, which can be mistaken for the main PV
fig A 1
Cavernous transformation of the PV. (Note also the small cyst at the porta, which does not demonstrate flow.)
Contrast angiography with arterioportography is considered to be the gold standard for assessing portal vein patency, but this technique is time-consuming and invasive and has similar results to carefully performed ultrasound. Ascites This is a transudate from the serosal surfaces of the gut, peritoneum and liver.
Splenomegaly This is the result of backpressure in the portal and splenic veins. The spleen can enlarge to six times its normal size. Varices These are venous anastomoses from the high-pressure portal system to the lower-pressure systemic circulation, which shunts the blood away from the portal system. These vessels have thinner walls than normal vessels, which makes them prone to bleeding.
Splenomegaly This is the result of backpressure in the portal and splenic veins. The spleen can enlarge to six times its normal size. Varices These are venous anastomoses from the high-pressure portal system to the lower-pressure systemic circulation, which shunts the blood away from the portal system. These vessels have thinner walls than normal vessels, which makes them prone to bleeding.
The common sites are:
● Gastric and lower oesophagus Oesophageal varices are particularly prone to bleeding and this is often the patient’s presenting symptom.
They are difficult to see on abdominal ultrasound because of overlying stomach and are better demonstrated with endoscopic
techniques. Left coronal scans may demonstrate tortuous vessels at the medial aspect of the upper pole of the spleen.
● Spleno-renal An anastomosis between the splenic and left renal veins which is often seen on ultrasound as a large, tortuous vessel at the
lower edge of the spleen (Fig. B, C). (These anastomoses are usually very efficient at and so these patients have a lower incidence of gastric varices and therefore a better prognosis.)
● Periumbilical A substantial vessel can often be seen in the liver lying in the ligamentum teres (Fig. D, E), and running down the anterior abdominal wall to a knot of vessels at the umbilicus, the so-called ‘caput medusae’. (A patent para-umbilical channel may occasionally be seen in normal patients, but
with a diameter of 1 or 2 mm.)
● Porta hepatis Varices around the main portal vein itself, especially if the latter is thrombosed (see below).
● Gallbladder wall Rarely, varices form around the gallbladder wall to bypass the main portal vein and feed into the intrahepatic portal branches (Fig.F).
● Gastric and lower oesophagus Oesophageal varices are particularly prone to bleeding and this is often the patient’s presenting symptom.
They are difficult to see on abdominal ultrasound because of overlying stomach and are better demonstrated with endoscopic
techniques. Left coronal scans may demonstrate tortuous vessels at the medial aspect of the upper pole of the spleen.
● Spleno-renal An anastomosis between the splenic and left renal veins which is often seen on ultrasound as a large, tortuous vessel at the
lower edge of the spleen (Fig. B, C). (These anastomoses are usually very efficient at and so these patients have a lower incidence of gastric varices and therefore a better prognosis.)
● Periumbilical A substantial vessel can often be seen in the liver lying in the ligamentum teres (Fig. D, E), and running down the anterior abdominal wall to a knot of vessels at the umbilicus, the so-called ‘caput medusae’. (A patent para-umbilical channel may occasionally be seen in normal patients, but
with a diameter of 1 or 2 mm.)
● Porta hepatis Varices around the main portal vein itself, especially if the latter is thrombosed (see below).
● Gallbladder wall Rarely, varices form around the gallbladder wall to bypass the main portal vein and feed into the intrahepatic portal branches (Fig.F).
Fig, B Ultrasound images
Cavernous transformation of the PV. (Note also the small cyst at
the porta, which does not demonstrate flow.
the porta, which does not demonstrate flow.
Fig. C ultrasound images The tortuous vessels of a spleno-renal shunt are demonstrated along the inferior border of the spleen.
fig D
Ultrasound images Large patent para-umbilical channel running along the ligamentum teres to the anterior abdominal wall in a patient with end-stage chronic liver disease and portal hypertension.
fig. E
Ultrasound images The para-umbilical vein culminates in a caput medusae just beneath the umbilicus.
fig. F
Ultrasound images Varices can be seen around the gallbladder wall in a case of hepatic fibrosis with portal hypertension.
LiveJournal Tags: Ultrasound images Portal hypertension









Post a Comment for "Ultrasound images Portal hypertension"