Intrahepatic
Clinical
A peripheral (intrahepatic) cholangiocarcinoma is probably more common than reported. Many are misdiagnosed as a hepatocellular carcinoma or even a benign neoplasm. Also, not all intrahepatic tumors can be clearly categorized into distinct hepatocellular or cholangiocellular origins. Some are even misdiagnosed as metastatic adenocarcinomas. Fine-needle biopsies simply reveal adenocarcinomatous tissue, and a correct diagnosis is made in only about half of these tumors, while in others a metastatic adenocarcinoma is suggested. Intrahepatic (peripheral) cholangiocarcinomas range from single to multicentric in origin. An occasional one grows intraluminally for varying lengths without major bile duct wall invasion. Also called a malignant papillary neoplasm, an intraductal component may or may not be identified by CT, depending on size.
Diffuse infiltration predominates in others and can eventually even lead to acute hepatic failure. These intrahepatic tumors tend not to invade portal venous branches, although an occasional one invades the portal vein and leads to portal hypertension.
The most common presentation is abdominal pain, weight loss, and malaise. Jaundice is absent unless a tumor invades and destroys sufficient liver parenchyma. An almost constant finding is an elevated serum alkaline phosphatase level. Most of these tumors are rather invasive and often progress rapidly; an exception is with those exhibiting an intraluminal papillary
growth pattern and these have a more indolent course.
Imaging, The use of earlier, less precise imaging suggested that with infiltrating tumors imaging could not suggest a specific diagnosis and that
imaging findings of most intrahepatic cholangiocarcinomas were similar to those seen with a hepatocellular carcinoma or metastasis. Yet a number of findings, albeit subtle, do suggest a biliary origin. Thus considerably dilated more proximal bile ducts, due to obstruction, are found in about half of patients with an intrahepatic cholangiocarcinoma. A patent portal vein branch passing through a tumor is generally considered a sign of a benign lesion; an intrahepatic cholangiocarcinoma, however, often also contains a patent portal vein branch. Also, in distinction to hepatocellular carcinomas,
most intrahepatic cholangiocarcinomas develop in a noncirrhotic liver. No capsule is identified. A few of these tumors develop calcifications. A minority grow primarily into the bile duct lumen. These intraluminal (papillary) intrahepatic bile duct carcinomas have rather nonspecific CT findings, but they are also associated with focal proximal intrahepatic bile duct dilation Cholangiography reveals obstruction and dilation of more peripheral bile ducts.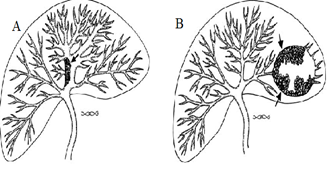
A peripheral (intrahepatic) cholangiocarcinoma is probably more common than reported. Many are misdiagnosed as a hepatocellular carcinoma or even a benign neoplasm. Also, not all intrahepatic tumors can be clearly categorized into distinct hepatocellular or cholangiocellular origins. Some are even misdiagnosed as metastatic adenocarcinomas. Fine-needle biopsies simply reveal adenocarcinomatous tissue, and a correct diagnosis is made in only about half of these tumors, while in others a metastatic adenocarcinoma is suggested. Intrahepatic (peripheral) cholangiocarcinomas range from single to multicentric in origin. An occasional one grows intraluminally for varying lengths without major bile duct wall invasion. Also called a malignant papillary neoplasm, an intraductal component may or may not be identified by CT, depending on size.
Diffuse infiltration predominates in others and can eventually even lead to acute hepatic failure. These intrahepatic tumors tend not to invade portal venous branches, although an occasional one invades the portal vein and leads to portal hypertension.
The most common presentation is abdominal pain, weight loss, and malaise. Jaundice is absent unless a tumor invades and destroys sufficient liver parenchyma. An almost constant finding is an elevated serum alkaline phosphatase level. Most of these tumors are rather invasive and often progress rapidly; an exception is with those exhibiting an intraluminal papillary
growth pattern and these have a more indolent course.
Imaging, The use of earlier, less precise imaging suggested that with infiltrating tumors imaging could not suggest a specific diagnosis and that
imaging findings of most intrahepatic cholangiocarcinomas were similar to those seen with a hepatocellular carcinoma or metastasis. Yet a number of findings, albeit subtle, do suggest a biliary origin. Thus considerably dilated more proximal bile ducts, due to obstruction, are found in about half of patients with an intrahepatic cholangiocarcinoma. A patent portal vein branch passing through a tumor is generally considered a sign of a benign lesion; an intrahepatic cholangiocarcinoma, however, often also contains a patent portal vein branch. Also, in distinction to hepatocellular carcinomas,
most intrahepatic cholangiocarcinomas develop in a noncirrhotic liver. No capsule is identified. A few of these tumors develop calcifications. A minority grow primarily into the bile duct lumen. These intraluminal (papillary) intrahepatic bile duct carcinomas have rather nonspecific CT findings, but they are also associated with focal proximal intrahepatic bile duct dilation Cholangiography reveals obstruction and dilation of more peripheral bile ducts.
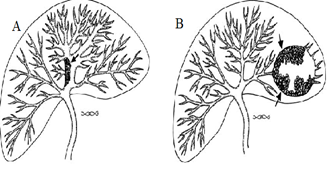
Radiology images of A: Diagram of intrahepatic cholangiocarcinoma (arrow) producing focal partial duct obstruction. B : A peripheral cholangiocarcinoma (arrows) has obstructed a left lobe duct resulting in a cavity mimicking an abscess.
Only a rare cholangiocarcinoma infiltrates diffusely without occluding bile duct. An occasional tumor manifests with an irregular bile duct lumen, displacement, and multicentric involvement mimicking primary intrahepatic
sclerosing cholangitis.
sclerosing cholangitis.
Radiology images of Intrahepatic cholangiocarcinoma. A: CT identifies dilated intrahepatic ducts containing stones in segment III. B: CT image 1 cm inferior to A shows a hypodense tumor anterior to the portal vein. C: Percutaneous transhepatic cholangiogram identifies the obstruction (arrow). Multiple stones are evident in the dilated ducts.
In most patients CT reveals a single, irregular, hypodense, nonencapsulated tumor of varying heterogeneity; contrast enhancement is generally evident, tending to be more pronounced in the tumor periphery, and, in fact, delayed postcontrast CT images are of value in differentiating an intrahepatic cholangiocarcinoma from a hepatocellular carcinoma. Hepatocellular carcinomas tend to have an early enhancement peak followed by a gradual
decrease, with the greatest tumor conspicuity during a delayed phase, several minutes after the start of contrast injection; on the other hand, with most cholangiocarcinomas the greatest conspicuity occurs during the portal
venous phase, and tumor attenuation increases during the delayed phase. Such prolonged contrast retention is probably related to the fibrotic matrix associated with many cholangiocarcino mas. Exceptions, however, do occur, and a rare cholangiocarcinoma is not definable during any dynamic CT imaging phase.
radiology images of Intrahepatic cholangiocarcinoma. Contrastenhanced CT identifies a poorly marginated tumor containing regions of necrosis (arrow). Dilated bile ducts are present in the medial segment of the left lobe and the right lobe.
Ultrasonography reveals either a single nodule having irregular margins or additional satellite nodules. Most tumors are hypoechoic, although some contain hyperechoic regions. Magnetic resonance imaging identifies intrahepatic cholangiocarcinomas as focal tumors, with some including a wedge-shape defect larger than the tumor itself, presumably secondary to surrounding edema and parenchymal compression, although an occasional infiltrating cholangiocarcinoma is intrinsically wedgeshaped. These tumors are mostly hypointense and occasionally isointense on T1- and variable in intensity on T2-weighted images; signal intensity on T2-weighted images depends mostly on the amount of fibrosis, necrosis, and secretions within the tumor. The occasional strongly hyperintense ones contain more secretions and necrosis. Postgadolinium enhancement varies considerably but often is progressive and moderate in extent and the intense immediate enhancement seen with many hepatocellular carcinomas is not evident. Postcontrast, some of these tumors show an enhancing rim, with progressive centrifugal filling of the tumor.
Some of these tumors encase adjacent vessels and result in focal liver atrophy and even a central scar. Central regions on T2-weighted images range from hypo- to hyperintense, with hypointensity reflecting fibrosis, a common finding with these tumors; postcontrast, these central hypointense regions range from homogeneous, to heterogeneous, to no enhancement, with fibrosis enhancing and necrotic regions not enhancing. None of the described findings is pathognomonic, and, with the exception of a dilated duct proximally, colorectal metastases often have a similar appearance. Adjacent noninvolved liver parenchyma is hyperintense on T1-weighted images; the high signal intensity is not suppressed with fat saturation, and this tissue enhances postcontrast, findings probably related to fibrosis. Preliminary evidence suggests that ferumoxides improves visualization of intrahepatic cholangiocarcinomas. An MRCP outlines bile ducts both proximal and distal to a tumor. Often multiple duct obstructions are detected. An MRCP can establish unresectability by showing extensive tumor spread.
Most of these tumors are hypovascular on angiography. Occasional arterioportal shunting is detected; a large tumor invades adjacent hepatic arteries and portal vein branches and can even invade the inferior vena cava. Hepatic artery invasion influences any planned resection, yet the accuracy of detecting hepatic artery invasion by CT and US is low. Multidetector CT angiography holds promise in detecting vascular invasion, but its specific role is not yet clear. Occasionally an intrahepatic cholangiocarcinoma contains foci of sarcomatous transformation. One such cholangiocarcinoma containing malignant fibrous histiocytoma like sarcomatous tissue was hypodense by CT; US showed a well-marginated, heterogeneous hypoechoic tumor, and MRI revealed a hypo- to isointense tumor on T1- and a heterogeneous appearance on T2-weighted images. The cholangiocarcinoma was hypovascular by angiography. Some of these sarcomatous tumors contain internal septa.
Therapy Of 61 patients with an intrahepatic cholangiocarcinoma seen at the Mayo Clinic over a 31- year period, 46% underwent resection for cure; survival at 3 years of those resected for cure was 60%. Survival of patients undergoing partial liver resection is significantly longer than of patients undergoing only drainage. An occasional patient survives long-term even if a tumor invades adjacent organs. An orthotopic liver transplantation is in an occasional patient with a slow performed growing tumor, but 3-year disease-free survival after transplantation is only in the teen percents. Arterial chemotherapy performed through an implanted port system appears to prolong survival of patients with unresectable intrahepatic cholangiocarcinomas.


Post a Comment for "Intrahepatic"