Non contrast CT Urology
Noncontrast scans are obtained to locate the kidneys, evaluate urolithiasis, detect acute hematoma, and obtain baseline density measurements of renal masses. Noncontrast CT is accepted as primary imaging to detect urinary calculi.
Contrast-enhanced CT Oral contrast medium
In the evaluation of urolithiasis, dense oral contrast medium in the bowel can make detection of ureteral stones more difficult . In addition, for 3-D CT angiography, positive oral contrast medium should not be given to improve postprocessing image quality and to avoid major overlay in postprocessed images. Some investigators suggest drinking 500 to 750 mL of water over a 15- to 20-minute period before the start of a renal CT examination .In CT angiography, the use of a saline chase bolus after contrast medium injection is essential to provide a compact contrast bolus and to push it toward the right atrium. The authors do not use
oral contrast medium for renal MDCT. Administration of intravenous contrast medium For the contrast-enhanced phases, the optimal timing depends on the volume of the contrast medium, the rate of its administration, and patients’ cardiac output. The difference between the start of contrast medium injection and the start of scanning is referred to as delay time. For specific vascular imaging studies, such as CT angiography, a fixed scanning delay is recommended, especially in patients who have cardiovascular disorders. If the delay is not chosen properly, the bolus may be missed completely with the short acquisition time. With MDCT, the delay time must be adjusted properly relative to patients’ contrast transit time. This can be determined easily using a test bolus injection or automatic bolus triggering. The test bolus technique requires the additional injection of a small amount of contrast medium (10–20 mL) before the acquisition of the CT angiography data, followed by the use of the same injection parameters (eg, flow rate). Using the bolus triggering (or bolus tracking) method, a region of interest is placed into the target vessel on an unenhanced image, and the attenuation level is monitored online within the region-of-interest during a single-level dynamic scan. Bolus tracking allows for the initial injection of the entire contrast medium volume, whereas the start of the data acquisition is triggered based on automated detection of the contrast bolus arrival using preassigned trigger thresholds (eg, 100–120 HU). The authors routinely use 100 to 120 mL of nonionic contrast at an infusion rate of 2 to 3 mL per second for routine renal imaging, 3 mL per second for CT urography, and 4 mL per second for CT angiography.
Contrast is injected through an 18-gauge angiocatheter placed in the antecubital vein followed by 250 mL of saline infusion to provide better visualization of the collecting system.
In the evaluation of urolithiasis, dense oral contrast medium in the bowel can make detection of ureteral stones more difficult . In addition, for 3-D CT angiography, positive oral contrast medium should not be given to improve postprocessing image quality and to avoid major overlay in postprocessed images. Some investigators suggest drinking 500 to 750 mL of water over a 15- to 20-minute period before the start of a renal CT examination .In CT angiography, the use of a saline chase bolus after contrast medium injection is essential to provide a compact contrast bolus and to push it toward the right atrium. The authors do not use
oral contrast medium for renal MDCT. Administration of intravenous contrast medium For the contrast-enhanced phases, the optimal timing depends on the volume of the contrast medium, the rate of its administration, and patients’ cardiac output. The difference between the start of contrast medium injection and the start of scanning is referred to as delay time. For specific vascular imaging studies, such as CT angiography, a fixed scanning delay is recommended, especially in patients who have cardiovascular disorders. If the delay is not chosen properly, the bolus may be missed completely with the short acquisition time. With MDCT, the delay time must be adjusted properly relative to patients’ contrast transit time. This can be determined easily using a test bolus injection or automatic bolus triggering. The test bolus technique requires the additional injection of a small amount of contrast medium (10–20 mL) before the acquisition of the CT angiography data, followed by the use of the same injection parameters (eg, flow rate). Using the bolus triggering (or bolus tracking) method, a region of interest is placed into the target vessel on an unenhanced image, and the attenuation level is monitored online within the region-of-interest during a single-level dynamic scan. Bolus tracking allows for the initial injection of the entire contrast medium volume, whereas the start of the data acquisition is triggered based on automated detection of the contrast bolus arrival using preassigned trigger thresholds (eg, 100–120 HU). The authors routinely use 100 to 120 mL of nonionic contrast at an infusion rate of 2 to 3 mL per second for routine renal imaging, 3 mL per second for CT urography, and 4 mL per second for CT angiography.
Contrast is injected through an 18-gauge angiocatheter placed in the antecubital vein followed by 250 mL of saline infusion to provide better visualization of the collecting system.
Phases of renal enhancement
There are four phases of renal enhancement. Arterial-phase imaging, performed to evaluate the arterial anatomy, is a short phase that occurs after a delay time of approximately 15 to 25 seconds. In the late arterial phase, the renal veins usually also opacify. The authors prefer a bolus-triggering method (aorta threshold value 120 HU) rather than a standard delay for arterial-phase imaging. The angionephrographic (corticomedullary or venous) phase, performed to evaluate the venous anatomy, begins approximately 30 to 40 seconds after the start of contrast medium injection and continues for approximately 60 seconds. In this
phase, intense enhancement of the renal cortex can be observed while the medulla remains relatively less
enhanced.
The nephrographic phase refers to the time during which the renal cortex and medulla are enhanced uniformly and contrast medium has not yet entered the renal collecting system. This phase begins 75 to 100 seconds after the start of contrast medium injection and is optimal for the detection of focal masses arising in the cortex or medulla and for evaluation of the renal parenchyma. The authors use a standard 100-second delay to obtain nephrographic-phase images of the kidney.
The delayed phase (the excretory or urographic phase), used to evaluate renal collecting system and ureters, begins 3 minutes after the start of contrast medium injection. In this phase, while the intensity of the nephrogram declines, excretion of the contrast medium permits opacification of the calyces, renal pelvises, and ureters. The authors obtain excretory-phase images at 10 minutes routinely.
There are four phases of renal enhancement. Arterial-phase imaging, performed to evaluate the arterial anatomy, is a short phase that occurs after a delay time of approximately 15 to 25 seconds. In the late arterial phase, the renal veins usually also opacify. The authors prefer a bolus-triggering method (aorta threshold value 120 HU) rather than a standard delay for arterial-phase imaging. The angionephrographic (corticomedullary or venous) phase, performed to evaluate the venous anatomy, begins approximately 30 to 40 seconds after the start of contrast medium injection and continues for approximately 60 seconds. In this
phase, intense enhancement of the renal cortex can be observed while the medulla remains relatively less
enhanced.
The nephrographic phase refers to the time during which the renal cortex and medulla are enhanced uniformly and contrast medium has not yet entered the renal collecting system. This phase begins 75 to 100 seconds after the start of contrast medium injection and is optimal for the detection of focal masses arising in the cortex or medulla and for evaluation of the renal parenchyma. The authors use a standard 100-second delay to obtain nephrographic-phase images of the kidney.
The delayed phase (the excretory or urographic phase), used to evaluate renal collecting system and ureters, begins 3 minutes after the start of contrast medium injection. In this phase, while the intensity of the nephrogram declines, excretion of the contrast medium permits opacification of the calyces, renal pelvises, and ureters. The authors obtain excretory-phase images at 10 minutes routinely.
Image processing and postprocessing techniques
Axial 3- to 5-mm, reconstructed slices are obtained to examine entire kidneys and the collecting system. The authors use a 3-mm slice thickness routinely for flank pain evaluation and a 5-mm slice thickness for nonspecific abdominal pain evaluation. The figures demonstrate the reconstructed images using the following techniques
Axial 3- to 5-mm, reconstructed slices are obtained to examine entire kidneys and the collecting system. The authors use a 3-mm slice thickness routinely for flank pain evaluation and a 5-mm slice thickness for nonspecific abdominal pain evaluation. The figures demonstrate the reconstructed images using the following techniques
MPR
CPR; note that the visualization of the ureter is facilitated
MIP;
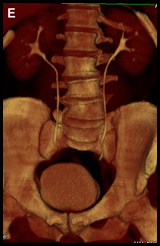
SSD;
VRT.
The smaller collimation allows better quality MPR of the renal parenchyma and collecting system. Four main 3-D visualization techniques currently are used on clinical 3-D workstations: MPR, maximum intensity projections (MIP), shaded surface displays (SSD), and a volume-rendering technique (VRT).
jurnal radiology Tags: Phases of renal enhancement, CT Scan of renal




Excellent blog very nice and unique information related to Beclovent. Thanks for sharing this information.
ReplyDeleteContrast media
Great information...Your post the very informative i have learned some information about your blog thank you for Sharing the great information.....Contrast media
ReplyDeleteThis was a useful post and I think it's fairly easy to see in the other reviews, so this post is well written and useful. Keep up the good work.contrast media radiology
ReplyDelete