Radiologic Evaluation of Malignant Pleural and Peritoneal Mesothelioma
Malignant mesothelioma is an asbestos-associated malignancy arising from the mesothelial cells of the pleural and peritoneal cavities, as well as the pericardium and the tunica vaginalis.
Mesothelioma usually presents in the fifth to seventh decades, and 70-80 % of cases occur in men (Moore et al., 2008). Malignant pleural mesothelioma (MPM) is the most widely form of mesothelioma. Patients frequently present with dyspnea, chest pain, cough, and weight loss (Moore et al., 2008, Wang et al., 2004). Although most of the mesotheliomas cover the pleural surface, approximately 35% arise only from peritoneum. Patients with malignant peritoneal mesothelioma may present with abdominal pain, distention, anorexia, and weight loss (Park et al., 2008).
Radiologic modalities play a crucial role in the evaluation of malignant mesothelioma. Computed tomography is the primary imaging method used for the diagnosis and the staging of malignant mesothelioma, but also for guiding biopsy for tissue diagnosis.
Magnetic resonans imaging (MRI) is useful for detection of extension of disease, especially to the chest wall and diaphragm (Moore et al., 2008, Wang et al., 2004). In this article we review radiologic findings of malignant pleural and peritoneal mesothelioma with our patient archives. We also wants to give some information about differential diagnosis malignant pleural and peritoneal mesothelioma.
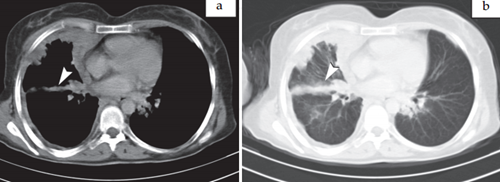
Mesothelioma images > Fig. 1. Axial contrast enhanced CT parenchymal (a.) and mediastinal sections (b.) shows
nodular, irregular and circumferantial right sided pleural thickening in 55 year-old man. Note that contracted right hemithorax and anterior mediastinal lymph node (arrow head). We can see pleural calcification on left sided pleural surface (arrow head).
Axial contrast enhanced CT mediastinal (a.) and parenchymal sections (b.) shows right sided irregular pleural thickening and right major fissur involvement (arrow head).
Axial non- contrast enhanced CT a milimetric parenchymal nodul in right middle lobe (arrow head)
Axial contrast enhanced CT show 1 cm paracardiac lymphadenopathy in 65 year old man with MPM.
Axial contrast enhanced CT shows pericardial invasion and pericardial effusion.
Intravenous contrast-enhanced CT is the primary imaging modality for suspected malignant mesothelioma. CT can show the whole pleural surface and diaphragm. CT findings that is seen mostly are nodular pleural thickening, unilateral pleural effusion, pleural calcification, thickening of interlobar fissur, reduction of thoracic volume (Wang et al., 2004, Ismail-Khan et al., 2006). Pleural calcification is seen approximately 20% of cases (Moore et al., 2008, Wang et al., 2004). Typically, both the visceral and parietal pleurae are involved. Malignant pleural thickening characteristically is circumferantial, nodular and > 1 cm. Also, mediastinal pleural involvement is often detected (Ismail-Khan et al., 2006). Malignant pleural mesothelioma is locally aggressive with invasion of the chest wall, mediastinum and diaphragm. Obliteration of extrapleural fat planes, invasion
of intercostal muscles, displacement of ribs, and bone destruction are findings of chest wall involvement. Heart, esophagus, trachea and major vascular structures of mediastinum may be involved by tumor. Nodular pericardial thickening and pericardial effusion refers to pericardial invasion by malignant pleural mesothelioma. Obliteration of surrounding fat planes of mediastinal organs, covering of vascular structure more than 50% is a strong evidence of invasion (Moore et al., 2008, Wang et al., 2004, Miller et al.,1996, Patz et al., 1992).
Pulmonary metastases of MPM presenting as nodules and masses and, rarely, diffuse miliary nodules may be seen at CT. Chest CT may also rarely demonstrate extrathoracic spread of MPM. Metastasis to the hilar and mediastinal lymph nodes is present at autopsy in approximately 40-45% of patients with MPM ( Miller et al., 1996, Patz et al., 1992, Dynes et al., 1992).
MRI screening is not used routinely in the assessment of malignant mesothelioma, however in patients with potentially resectable disease, MRI can help to provide additional staging information over and above CT. Using gadolinium enhancement, MRI can advance the identification of tumor extension into the diaphragm or chest wall. MRI also is preferred in some patients whom intravenous iodinated contrast is contraindicated.
Malignant pleural mesothelioma is typically isointense or slightly hyperintense on T1-weighted images and moderately hyperintense on T2-weighted images relative to adjacent chest wall muscle. After the gadolinium injection, MPM shows enhancement. MR imaging is superior to CT for showing invasion of the diaphragm and invasion of endothoracic fascia or a single chest wall focus (Moore et al., 2008, Miller et al., 1996, Patz et al., 1992).
The radiologic differential diagnosis includes metastatic pleural disease, pleural lymphoma, asbestos releated benign pleural disease, and tuberculous empyema. Pleural rind, nodular pleural thickening, pleural thickening greater than 1 cm, and mediastinal pleural involvement favor malignant pleural disease. Pleural calsification is usually seen in benign process. Mesothelioma can not be distinguished from metastatic pleural disease on CT.
Discrimination between epithelial types of mesothelioma and metastatic adenocarcinoma requires histochemical, immunohistochemical, and ultrastructural analysis. The presence of hilar-mediastinal adenopathy may be helpful in differentiating metastases and lymphoma from mesothelioma. The radiologic criteria for unresectability are tumor encasing diaphragm, invasion of extrapleural soft tissue, infiltration, displacement, or seperation of ribs by tumor, or bone destruction (Moore et al., 2008, Dynes et al., 1992, Barreiro et al., 2006, Jeong et al., 2008).
Morphologically malignant pleural mesothelioma can be seen in three forms: epithelial, sarcomatous, and mixed. The mixed form is usually mentioned as biphasic or bimorphic. Mixed tumors are composed of both epithelial and sarcomatous components. Epithelial mesotheliomas have a better diagnosis than sarcomatous and mixed tumors so differential diagnosis is very important for determining the prognosis. Epithelial malignant mesotheliomas consist of cells that are similar to normal mesothelial cells. The cells form a tubulopapillary or trabecular pattern. Epithelial malignant mesothelioma may also show prominent secretory changes, microglandular patterns, signet cell structure, or desmoplastic responses that make these tumors difficult to differentiate from adenocarcinomas based on routine histologic analysis alone. The sarcomatous pattern of malignant mesothelioma is typically consist of closely packed spindle cells. No immunohistochemical markers are spesific for malignant mesotheliomas and so there are some immunohistochemical markers such as calretinin thrombomodulin, and cytokeratin 5/6 to differentiate from metastatic adenocarcinomas and soft tissue sarcomas that have similar to histologic appearances (Levy et al., 2008).




I was diagnosed as HEPATITIS B carrier in 2013 with fibrosis of the
ReplyDeleteliver already present. I started on antiviral medications which
reduced the viral load initially. After a couple of years the virus
became resistant. I started on HEPATITIS B Herbal treatment from
ULTIMATE LIFE CLINIC (www.ultimatelifeclinic.com) in March, 2020. Their
treatment totally reversed the virus. I did another blood test after
the 6 months long treatment and tested negative to the virus. Amazing
treatment! This treatment is a breakthrough for all HBV carriers.