Interventional Ultrasound Therapeutic Aspiration and Drainage
Preparations and Technique
Prerequisites: Quick PT i 70%, platelets i 100000/mm3. Factor analysis (e.g., factor XIII) may be indicated in patients with a hematologic systemic disease. Obtain informed consent.
Setup (Fig. 77):
x Skin prep, sterile drapes, local anesthesia, razor, scalpel blade
x Drainage materials: Small-gauge catheters (F 8) are often adequate for cyst
aspiration. Abscess drainage requires a larger (double-lumen) suction-irrigation
catheter (F 14).
x Suture material (plus scissors and needle holder)
x Dressing materials
x Skin prep, sterile drapes, local anesthesia, razor, scalpel blade
x Drainage materials: Small-gauge catheters (F 8) are often adequate for cyst
aspiration. Abscess drainage requires a larger (double-lumen) suction-irrigation
catheter (F 14).
x Suture material (plus scissors and needle holder)
x Dressing materials
Materials for Seldinger drainage.
1añc Puncture needle (a), stylet (b), and depth-setting lock screw
(c). 2 Guidewire, 3 dilators, 4 pigtail catheter, F 8 (e.g., for cyst drainage)
1añc Puncture needle (a), stylet (b), and depth-setting lock screw
(c). 2 Guidewire, 3 dilators, 4 pigtail catheter, F 8 (e.g., for cyst drainage)
Procedure for percutaneous drainage (Seldinger technique): x Define the target lesion and puncture route, and measure as for a diagnostic aspiration (Figs 78, 79a). Make a stab incision with a scalpel blade.
x Insert the needle, remove the stylet, and check the position of the needle tip echo (may be necessary to aspirate and instill saline solution). Introduce the guidewire and remove the puncture needle. Dilate the tract with graded dilators, and introduce the drainage cathete r (Fig. 79b). Remove the guidewire and check catheter position (may be done radiographically). Secure the catheter with sutures and apply a dressing.
x Insert the needle, remove the stylet, and check the position of the needle tip echo (may be necessary to aspirate and instill saline solution). Introduce the guidewire and remove the puncture needle. Dilate the tract with graded dilators, and introduce the drainage cathete r (Fig. 79b). Remove the guidewire and check catheter position (may be done radiographically). Secure the catheter with sutures and apply a dressing.
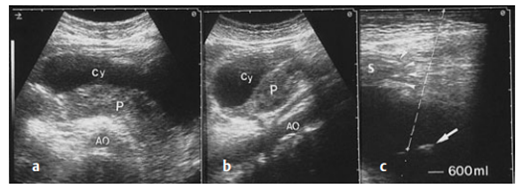
Diagnostic and therapeutic aspiration. a B-mode image shows an anechoic pancreatic pseudocyst anterior to the pancreas (P). AO = aorta.
b Longitudinal scan of the pseudocyst (Cy). c The angle of the puncture is carefully planned to bypass the stomach (arrow heads). Large arrow: needle tip echo
b Longitudinal scan of the pseudocyst (Cy). c The angle of the puncture is carefully planned to bypass the stomach (arrow heads). Large arrow: needle tip echo
Therapeutic catheter drainage. a Large, rounded, sharply circumscribed, intrasplenic cystic mass with fluctuating internal echoes on real-time examination. b The liquid mass was drained externally using Seldinger technique.
The arrows indicate the catheter in place. c Follow-up scan several months after catheter drainage shows complete resolution of the cystic lesion, leaving a calcified scar. SP = spleen, CY = cystic lesion, S = acoustic shadow.
The arrows indicate the catheter in place. c Follow-up scan several months after catheter drainage shows complete resolution of the cystic lesion, leaving a calcified scar. SP = spleen, CY = cystic lesion, S = acoustic shadow.
Indications and Guidelines for Specific Lesions
Pseudocysts (e.g., of the pancreas): x Therapeutic procedure: See Fig. bellow).
Algorithm for the management of pancreatic pseudocysts (after Schwerk)
x Technique: See Figs. bellow
Ultrasound-guided percutaneous external drainage of pancreatic pseudocysts (after Schwerk). a Transhepatic (or transgastric) fine-needle aspiration. AO = aorta, L = liver, P = pancreas. b External catheter drainage using Seldinger technique. The guidewire is advanced into the pseudocyst under sonographic guidance, avoiding the perforation of internal organs. c Transgastric
external catheter drainage.
external catheter drainage.
Abscesses (of the liver or spleen, intra- or retroperitoneal, subphrenic):
Abscesses (of the liver or spleen, intra- or retroperitoneal, subphrenic):
x The treatment of choice is repeated percutaneous drainage or therapeutic catheter drainage.
Note: Irrigate the abscess cavity with saline solution. Drains should be flushed once or twice daily to prevent clogging.
x The treatment of choice is repeated percutaneous drainage or therapeutic catheter drainage.
Note: Irrigate the abscess cavity with saline solution. Drains should be flushed once or twice daily to prevent clogging.
n Primary symptomatic cysts:
x By definition, these lesions are lined with potentially secretory epithelium.
x If the contents reaccumulate after percutaneous drainage, the cyst should be surgically extirpated or evacuated by catheter drainage followed by the injection of pure alcohol (99.5 %). Catheter placement should be checked radiographically.
x Percutaneous drainage may be combined with sclerotherapy for cysts of the
liver, spleen, kidney, etc.
Empyema: Intrathoracic, gallbladder, ascites, pleural effusion, pericardial effusion.
x By definition, these lesions are lined with potentially secretory epithelium.
x If the contents reaccumulate after percutaneous drainage, the cyst should be surgically extirpated or evacuated by catheter drainage followed by the injection of pure alcohol (99.5 %). Catheter placement should be checked radiographically.
x Percutaneous drainage may be combined with sclerotherapy for cysts of the
liver, spleen, kidney, etc.
Empyema: Intrathoracic, gallbladder, ascites, pleural effusion, pericardial effusion.
Contraindications:
Refusal of informed consent or lack of patient cooperation Coagulation disorder
Unsafe drainage route
Specific Types of Therapeutic Drainage
Alcohol instillation:
x Indications: Malignant tumors (e.g., malignant primary or secondary hepatic
tumors), thyroid adenoma.
x Prerequisites: Good visualization, solitary lesion, tumor I 5 cm
x Indications: Malignant tumors (e.g., malignant primary or secondary hepatic
tumors), thyroid adenoma.
x Prerequisites: Good visualization, solitary lesion, tumor I 5 cm
x Prerequisites: Good visualization, solitary lesion, tumor I 5 cm.
n Suprapubic bladder catheter:
x Indication: Incontinence that necessitates long-term urinary diversion. Possible causes include outflow obstruction due to inoperable prostatic carcinoma.
x In principle, suprapubic aspiration of a full bladder can be carried out after clinical palpation and percussion. Ultrasound-guided aspiration is recommended only when the bladder volume is small
n Suprapubic bladder catheter:
x Indication: Incontinence that necessitates long-term urinary diversion. Possible causes include outflow obstruction due to inoperable prostatic carcinoma.
x In principle, suprapubic aspiration of a full bladder can be carried out after clinical palpation and percussion. Ultrasound-guided aspiration is recommended only when the bladder volume is small
Percutaneous nephrostomy:
x Indication: Ultrasound-guided puncture aided by fluoroscopy is appropriate for renal pelvic dilatation that is clearly demonstrated by sonography.
x Indication: Ultrasound-guided puncture aided by fluoroscopy is appropriate for renal pelvic dilatation that is clearly demonstrated by sonography.
x Technique: Using the Seldinger technique, a needle is passed into the dilated calyx under continuous sonographic guidance from a posterolateral approach, avoiding the vascularized renal medulla. The tract is dilated, and a pigtail catheter (F 5–8) is introduced.
Interpretation
Pancreatic pseudocysts:
x Success rate: 60–90% depending on the location, size, and consistency of the pseudocyst
x Complications: Bleeding, septicemia, organ injuries in 5–10 % of cases. The complication rate can be lowered by finding a safe drainage route that avoids parenchymatous organs, gastrointestinal structures and the costophrenic angle.
x Success rate: 60–90% depending on the location, size, and consistency of the pseudocyst
x Complications: Bleeding, septicemia, organ injuries in 5–10 % of cases. The complication rate can be lowered by finding a safe drainage route that avoids parenchymatous organs, gastrointestinal structures and the costophrenic angle.
Abscesses:
x Success rate: 80–95 %
x Complications: With a safe access route and proper instrumentation, the complication rate is approximately 10% (sepsis, bleeding, pleural empyema, fistula formation).
x Success rate: 80–95 %
x Complications: With a safe access route and proper instrumentation, the complication rate is approximately 10% (sepsis, bleeding, pleural empyema, fistula formation).
Primary symptomatic cysts:
x Success rate: i 95%
x Complication rate: I 5% (infection, bleeding)
x Success rate: i 95%
x Complication rate: I 5% (infection, bleeding)
Empyema:
x Success rate: 72–88 % with early diagnosis of pleural empyema
x Complication rate: Low (bleeding from intercostal vessels)
x Success rate: 72–88 % with early diagnosis of pleural empyema
x Complication rate: Low (bleeding from intercostal vessels)
Nephrostomy:
x Success rate: 95%
x Complication rate: 5% (bleeding, infection)
x Success rate: 95%
x Complication rate: 5% (bleeding, infection)




Post a Comment for "Interventional Ultrasound Therapeutic Aspiration and Drainage"