Abdominal Tuberculosis
Clinical
An increasing prevalence is evident not only for pulmonary tuberculosis but also for its extrapulmonary manifestation. Isolated abdominal involvement is not uncommon in endemic regions. Fatigue, prolonged fever, weight loss, nonspecific bowel symptoms, and a chronic wasting illness are common clinical findings. An erroneous initial diagnosis is common in parts of the world with a low prevalence of abdominal tuberculosis. Hypercalcemia developed in patients with tuberculous peritonitis without pulmonary involvement. Elevated serum CA 125 tumor marker levels are found in some of these patients; levels decrease after antituberculous therapy.
Tuberculosis ranges from disseminated disease to abdominal involvement only.Abdominal tuberculosis varies in organ involvemen considerably, with ulcerative ileocecal involvement not uncommon. Peritonitis, mesenteric and extraperitoneal lymphadenopathy, and genitourinary involvement can occur as separate findings or together; multiorgan involvement, including ulcerative ileocecal involvement is not uncommon. Bowel perforation and obstruction lead to an acute abdomen. Presence vascular and perivascular granulomas, intraluminal thrombi and subintimal fibrosis suggest that bowel ischemia is a common pathway.
A diagnosis of peritoneal tuberculosis is difficult; in spite of clinical, endoscopic, and radiologic evaluation, peritoneal tuberculosis, especially if it involves the ileocecal region, is readily misdiagnosed as Crohn’s disease.Differentiating peritoneal tuberculosis from advanced ovarian cancer is difficult. Malignant lymphoma is also often in the differential diagnosis. Tuberculous ascitic fluid acid-fast stains tend to be negative and not all Mycobacterium tuberculosis cultures are positive. Biopsy in some patients reveals epithelioid giant-cell granulomas containing caseous necrosis.At times diagnostic laparotomy and culture of tissue biopsy specimens are necessary for diagnosis.
Imaging
Imaging identifies intra- and extraperitoneal lymphadenopathy. At times these enlarged nodes are focal in location and mimic a malignancy. Nevertheless, CT lymph node location and specific node appearance provide clues aiding the differentiation of these two entities. Tuberculosis tends to involve more superior para-aortic lymph nodes, while lymphoma more often involves the inferior para-aortic lymph nodes. An exception is with disseminated tuberculosis, which affects nodes diffusely and involves the hepatoduodenal and hepatogastric ligaments and mesenteric and extraperitoneal lymph nodes; nondisseminated tuberculosis can involve similar node chains, except the inferior extraperitoneal lymph nodes are mostly spared. The large, confluent lymph nodes found in lymphoma are unusual with tuberculosis. An enlarged isolated lymph node chain is nonspecific; for instance, periportal adenopathy, detected by CT, can be an isolated manifestation of tuberculous adenitis, but the differential diagnosis also includes not only malignancies but also such benign diseases as sarcoidosis. Enlarged tuberculous lymph nodes tend toward a lower CT density than lymphomatous nodes. In tuberculous peritonitis a low-density center was seen in some enlarged nodes, and calcification eventually develop in a minority; the low-density portion probably represents caseation necrosis. Even more striking is peripheral rim contrast-enhancement with tuberculosis; lymphomatous nodes are more homogeneous in their enhancement.
Fine peritoneal septations are common in tuberculosis, and ascites is often enclosed in a lattice-like mesh. Tuberculous ascites tends to have a higher density than most ascitic fluid. Diffuse peritoneal thickening and infiltration of the greater omentum is common. In general, CT and US reveal similar findings, although bowel wall thickening is probably better appreciated with CT.At times CT and US complement each other in patients with suspected tuberculous peritonitis. With pelvic involvement the CT appearance often mimics a malignancy. An abdominal cocoon-like appearance can be associated with tuberculous pelvic involvement. Ultrasonography reveals a hyperechoic, thickened mesentery, mesenteric adenopathy, and less often dilated small bowel loops, minor ascites, and occasional omental thickening. A cone-shaped, contracted cecum and a dilated, edematous terminal ileum are diagnostic findings in the dry type of ileocecal tuberculosis.
An increasing prevalence is evident not only for pulmonary tuberculosis but also for its extrapulmonary manifestation. Isolated abdominal involvement is not uncommon in endemic regions. Fatigue, prolonged fever, weight loss, nonspecific bowel symptoms, and a chronic wasting illness are common clinical findings. An erroneous initial diagnosis is common in parts of the world with a low prevalence of abdominal tuberculosis. Hypercalcemia developed in patients with tuberculous peritonitis without pulmonary involvement. Elevated serum CA 125 tumor marker levels are found in some of these patients; levels decrease after antituberculous therapy.
Tuberculosis ranges from disseminated disease to abdominal involvement only.Abdominal tuberculosis varies in organ involvemen considerably, with ulcerative ileocecal involvement not uncommon. Peritonitis, mesenteric and extraperitoneal lymphadenopathy, and genitourinary involvement can occur as separate findings or together; multiorgan involvement, including ulcerative ileocecal involvement is not uncommon. Bowel perforation and obstruction lead to an acute abdomen. Presence vascular and perivascular granulomas, intraluminal thrombi and subintimal fibrosis suggest that bowel ischemia is a common pathway.
A diagnosis of peritoneal tuberculosis is difficult; in spite of clinical, endoscopic, and radiologic evaluation, peritoneal tuberculosis, especially if it involves the ileocecal region, is readily misdiagnosed as Crohn’s disease.Differentiating peritoneal tuberculosis from advanced ovarian cancer is difficult. Malignant lymphoma is also often in the differential diagnosis. Tuberculous ascitic fluid acid-fast stains tend to be negative and not all Mycobacterium tuberculosis cultures are positive. Biopsy in some patients reveals epithelioid giant-cell granulomas containing caseous necrosis.At times diagnostic laparotomy and culture of tissue biopsy specimens are necessary for diagnosis.
Imaging
Imaging identifies intra- and extraperitoneal lymphadenopathy. At times these enlarged nodes are focal in location and mimic a malignancy. Nevertheless, CT lymph node location and specific node appearance provide clues aiding the differentiation of these two entities. Tuberculosis tends to involve more superior para-aortic lymph nodes, while lymphoma more often involves the inferior para-aortic lymph nodes. An exception is with disseminated tuberculosis, which affects nodes diffusely and involves the hepatoduodenal and hepatogastric ligaments and mesenteric and extraperitoneal lymph nodes; nondisseminated tuberculosis can involve similar node chains, except the inferior extraperitoneal lymph nodes are mostly spared. The large, confluent lymph nodes found in lymphoma are unusual with tuberculosis. An enlarged isolated lymph node chain is nonspecific; for instance, periportal adenopathy, detected by CT, can be an isolated manifestation of tuberculous adenitis, but the differential diagnosis also includes not only malignancies but also such benign diseases as sarcoidosis. Enlarged tuberculous lymph nodes tend toward a lower CT density than lymphomatous nodes. In tuberculous peritonitis a low-density center was seen in some enlarged nodes, and calcification eventually develop in a minority; the low-density portion probably represents caseation necrosis. Even more striking is peripheral rim contrast-enhancement with tuberculosis; lymphomatous nodes are more homogeneous in their enhancement.
Fine peritoneal septations are common in tuberculosis, and ascites is often enclosed in a lattice-like mesh. Tuberculous ascites tends to have a higher density than most ascitic fluid. Diffuse peritoneal thickening and infiltration of the greater omentum is common. In general, CT and US reveal similar findings, although bowel wall thickening is probably better appreciated with CT.At times CT and US complement each other in patients with suspected tuberculous peritonitis. With pelvic involvement the CT appearance often mimics a malignancy. An abdominal cocoon-like appearance can be associated with tuberculous pelvic involvement. Ultrasonography reveals a hyperechoic, thickened mesentery, mesenteric adenopathy, and less often dilated small bowel loops, minor ascites, and occasional omental thickening. A cone-shaped, contracted cecum and a dilated, edematous terminal ileum are diagnostic findings in the dry type of ileocecal tuberculosis.
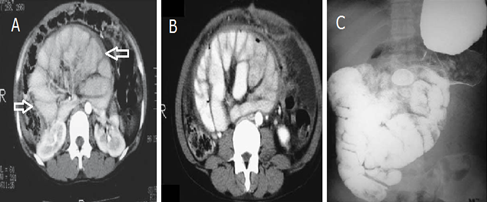
This is radiology images of the Abdominal tuberculosis manifesting as an abdominal cocoon. A,B: CT reveals small bowel within a thickened, enhancing sac (arrows). C: Small bowel barium study also shows nondilated bowel encased in a “sac.” Surgical biopsies identified peritoneal tubercles and omental lymph nodes containing caseating granulomas.
My name is hoover, my 18 year old daughter, Tricia was diagnosed with herpes 3 years ago. Since then, we have moved from one hospital to another. We tried all kinds of pills, but every effort to get rid of the virus was futile. The bubbles continued to reappear after a few months. My daughter was using 200mg acyclovir pills. 2 tablets every 6 hours and 15g of fusitin cream. and H5 POT. Permanganate with water to be applied twice a day, but all still do not show results. So, I was on the internet a few months ago, to look for other ways to save my only son. Only then did I come across a comment about the herbal treatment of Dr Imoloa and decided to give it a try. I contacted him and he prepared some herbs and sent them, along with guidance on how to use them via the DHL courier service. my daughter used it as directed by dr imoloa and in less than 14 days, my daughter recovered her health. You should contact dr imoloa today directly at his email address for any type of health problem; lupus disease, mouth ulcer, mouth cancer, body pain, fever, hepatitis ABC, syphilis, diarrhea, HIV / AIDS, Huntington's disease, back acne, chronic kidney failure, addison's disease, chronic pain, Crohn's pain, cystic fibrosis, fibromyalgia, inflammatory Bowel disease, fungal nail disease, Lyme disease, Celia disease, Lymphoma, Major depression, Malignant melanoma, Mania, Melorheostosis, Meniere's disease, Mucopolysaccharidosis, Multiple sclerosis, Muscular dystrophy, Rheumatoid arthritis Alzheimer's disease, parkinson's disease, vaginal cancer, epilepsy Anxiety Disorders, Autoimmune Disease, Back Pain, Back Sprain, Bipolar Disorder, Brain Tumor, Malignant, Bruxism, Bulimia, Cervical Disc Disease, Cardiovascular Disease, Neoplasms , chronic respiratory disease, mental and behavioral disorder, Cystic Fibrosis, Hypertension, Diabetes, Asthma, Autoimmune inflammatory media arthritis ed. chronic kidney disease, inflammatory joint disease, impotence, alcohol spectrum feta, dysthymic disorder, eczema, tuberculosis, chronic fatigue syndrome, constipation, inflammatory bowel disease. and many more; contact him at drimolaherbalmademedicine@
ReplyDelete