Mucinous Cystic Neoplasms of Pancreas
Clinical A distinction is often made between mucinous cystic neoplasms and intraductal mucinous tumors a tenuous and somewhat arbitrary differentiation based more on clinical and radiologic findings and tumor location than on pathologic grounds. From a simplistic viewpoint, mucinous cystic neoplasms do not communicate with the pancreatic ducts while intraductal mucinous tumors do communicate. Yet even this definition is not satisfactory. Most mucinous cystic neoplasms consist of a cystic septa-containing tumor and no pancreatic duct dilation unless obstructed by the tumor, while intraductal papillary mucinous tumors are small and lobulated assuming they are visualized at all and a major finding with them is a dilated main or branch pancreatic duct containing exuberant mucus.
Mucinous cystic neoplasms of the pancreas range from benign (cystadenoma) to malignant (cystadenocarcinoma), with an occasional tumor labeled borderline malignant. A cystadenoma is considered to be premalignant. These tumors range from unilocular to multilocular and their size varies considerably; their cavities are filled with mucin. Pancreatic body and tail are preferred sites. The malignant variety quite often obstructs the pancreatic duct. Tumor aspiration usually simply reveals mucin. A preponderance of these neoplasms occurs in middle-aged women.
A not uncommon occurrence is a cystadenocarcinoma initially misdiagnosed as a pseudocyst and the cyst then marsupialized to the stomach; the tumors true nature is realized only later when liver metastases are detected. A review of patients with this tumor revealed an overall 5-year survival rate for resectableones of 83%, and for those with infiltration limited to the pancreatic parenchyma, 74%; but this survival rate is only 28% if infiltration extends to other organs.
Mucinous cystic neoplasms of the pancreas range from benign (cystadenoma) to malignant (cystadenocarcinoma), with an occasional tumor labeled borderline malignant. A cystadenoma is considered to be premalignant. These tumors range from unilocular to multilocular and their size varies considerably; their cavities are filled with mucin. Pancreatic body and tail are preferred sites. The malignant variety quite often obstructs the pancreatic duct. Tumor aspiration usually simply reveals mucin. A preponderance of these neoplasms occurs in middle-aged women.
A not uncommon occurrence is a cystadenocarcinoma initially misdiagnosed as a pseudocyst and the cyst then marsupialized to the stomach; the tumors true nature is realized only later when liver metastases are detected. A review of patients with this tumor revealed an overall 5-year survival rate for resectableones of 83%, and for those with infiltration limited to the pancreatic parenchyma, 74%; but this survival rate is only 28% if infiltration extends to other organs.
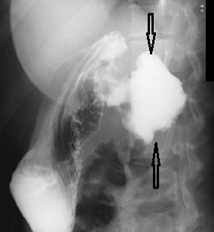
Radiology images of pancreatic cystadenoma (arrows) communicating with stomach. This patient was believed to have a pseudocyst, which was anastomosed to the stomach.
Imaging Imaging reveals one or more cysts; typically these cysts are fewer but larger than seen with serous tumors. Ultrasonography reveals a unilocular or,more often, a multilocular anechoic tumor, with tumor excrescences and debris modifying this appearance. Endoscopic US better evaluates their complex structure. Thus the number of cysts and cyst size are useful criteria in differentiating between the microcystic (serous) and macrocystic (mucinous)
tumors. Using criteria that a mucinouscystic neoplasm should contain fewer than six cysts having a diameter of >2cm, out of 17 mucinous cystadenomas and cystadenocarcinomas US correctly diagnosed 88%.
This is radiology images of mucinous cystadenoma. A: Transverse US identifies multiple pancreatic cysts (arrow), including one in the tail (arrowhead) (A, aorta; V, vena cava). B: CT reveals superior mesenteric artery (a) and vein (v) encased by tumor. C: A scan inferior to that in part B identifies a pancreatic tail cyst (arrowhead) (a, aorta; v, vena cava).
Soft tissue nodules project into some of these cysts. Septations tend to be thicker than those seen with microcystic neoplasms. An occasional tumor develops calcifications that are seen with both benign and malignant tumors. Local invasion is evident with some carcinomas. Occasionally these tumors are first detected through liver metastases. Thus a large calcified tumor in the body and tail occasionally manifests its malignant nature with multiple liver tumors.
An MRI identifies multilocular or unilocular cysts having a relatively thick wall. The cysts tend toward hyperintensity on T1- weighted sequences, presumably due to their high mucin content, and are, as expected for nonflowing fluid, hyperintense on T2-weighted images. Those tumors containing more mucin have a higher MR T1-weighted signal intensity than those containing more watery fluid; tumors containing gelatinous mucin tend to bemalignant, while those containing more watery fluid tend to be benign. The cysts do not enhance postcontrast.
Benign and malignant tumor varieties have a similar imaging appearance, although thick septa and nodularity point toward malignancy. Invasion of adjoining structures or metastasis signifies malignancy. An FDG-PET detected only 59% of 22 mucinous carcinomas, with an inverse correlation with the amount of tumor mucin.
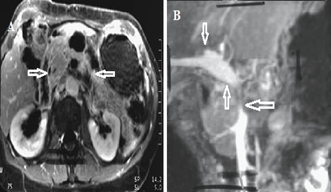
Radiology images of mucinous cystic adenocarcinoma. A: A contrast-enhanced MRI reveals a tumor containing solid and cystic components (arrows).B: Magnetic resonance angiography (MRA) identifies a narrowed superior mesenteric vein (arrow),patent portal vein (arrowheads) and nonvisualization of an occluded splenic vein.

Post a Comment for "Mucinous Cystic Neoplasms of Pancreas"