Colocolic intussusception
Gastrointestinal tract images In an intussusception, a segment of bowel, the intussusceptum, invaginates into the lumen of an adjacent intussuscipiens. Any part of bowel can intussuscept, although a mobile intraperitoneal bowel loop and its associated mesentery are most often involved. The intussusceptum usually invaginates distally, although occasional proximal invagination does occur (for example, a jejunogastric intussusception after a Billroth II operation). Intussusceptions range from transient to fixed. As discussed below, some are reduced with pressure. By its bulk, an intussusception should obstruct the bowel lumen, although in distinction to pediatric patients, bowel obstruction is not a prominent feature of adult intussusceptions. A more serious consequence, especially in the younger patient, is vascular occlusion of the intussusceptum, generally venous, and resultant ischemia.
Adults
Intussusceptions in most adults have an identifiable lead point and range from enteroenteric, to ileocolic, to colocolic, to rectal prolapse. The most common lead point is a cecal adenocarcinoma; less common is cecal lymphoma or a benign polyp. Rarer lead points in adults consist of pseudomembranous colitis, Meckel’s diverticulum, a rare duplication, endometrioma, or even calcified cecal fecaliths. An appendiceal polyp in a patient with Peutz-Jeghers syndrome acted as a lead point for intussusception. Although most colonic lipomas are intramural and sessile, they are prone to becoming pedunculated and act as lead points for an intussusception. Not all of these are at the ileocecal region; a number of sigmoid lipoma-associated sigmoidorectal
intussusceptions have been reported. A rectal intussusception is usually a transient phenomenon occurring during straining, is idiopathic, and is associated with constipation. Proctography shows circular infolding of the rectal wall during straining. The criteria defining when such infolding is abnormal are not well established, and minor changes probably are best considered normal variants, but solitary rectal ulcer syndrome (discussed later) is in the differential diagnosis. Computed tomography and MR detect most adult ileocolic intussusceptions but, aside from a lipoma, identification of a lead point is difficult. At times even endoscopic biopsy fails to provide an etiology, and the diagnosis is established only after a right hemicolectomy.
Computed tomography findings of an intussusception consist of a target or sausage-shaped inhomogeneous soft tissue tumor. The appearance varies depending on the relative orientation of the x-ray beam and intussusception. Colocolic intussusceptions caused by a colonic lipoma can be suggested by US; CT is diagnostic if fat is detected in the lead point, although the lack of fat in the lead point due to infarction and necrosis of an intussuscepted tumor does not exclude a lipoma. Unenhanced CT has a role if ischemia is suspected in adults with an intussusception; CT findings of a hypodense layer in the intussusceptum or surrounding fluid or gas should suggest vascular compromise; lumen obstruction is not always present in an ischemic or necrotic intussusception.
Overlying pneumatosis cystoides intestinalis and enteritis cystica profunda are uncommon associated finding of a colocolic intussusception. Magnetic resonance imaging also readily identifies intussusceptions, with findings similar to those found with CT. Magnetic resonance imaging reveals concentric bowel rings.
Intussusceptions in most adults have an identifiable lead point and range from enteroenteric, to ileocolic, to colocolic, to rectal prolapse. The most common lead point is a cecal adenocarcinoma; less common is cecal lymphoma or a benign polyp. Rarer lead points in adults consist of pseudomembranous colitis, Meckel’s diverticulum, a rare duplication, endometrioma, or even calcified cecal fecaliths. An appendiceal polyp in a patient with Peutz-Jeghers syndrome acted as a lead point for intussusception. Although most colonic lipomas are intramural and sessile, they are prone to becoming pedunculated and act as lead points for an intussusception. Not all of these are at the ileocecal region; a number of sigmoid lipoma-associated sigmoidorectal
intussusceptions have been reported. A rectal intussusception is usually a transient phenomenon occurring during straining, is idiopathic, and is associated with constipation. Proctography shows circular infolding of the rectal wall during straining. The criteria defining when such infolding is abnormal are not well established, and minor changes probably are best considered normal variants, but solitary rectal ulcer syndrome (discussed later) is in the differential diagnosis. Computed tomography and MR detect most adult ileocolic intussusceptions but, aside from a lipoma, identification of a lead point is difficult. At times even endoscopic biopsy fails to provide an etiology, and the diagnosis is established only after a right hemicolectomy.
Computed tomography findings of an intussusception consist of a target or sausage-shaped inhomogeneous soft tissue tumor. The appearance varies depending on the relative orientation of the x-ray beam and intussusception. Colocolic intussusceptions caused by a colonic lipoma can be suggested by US; CT is diagnostic if fat is detected in the lead point, although the lack of fat in the lead point due to infarction and necrosis of an intussuscepted tumor does not exclude a lipoma. Unenhanced CT has a role if ischemia is suspected in adults with an intussusception; CT findings of a hypodense layer in the intussusceptum or surrounding fluid or gas should suggest vascular compromise; lumen obstruction is not always present in an ischemic or necrotic intussusception.
Overlying pneumatosis cystoides intestinalis and enteritis cystica profunda are uncommon associated finding of a colocolic intussusception. Magnetic resonance imaging also readily identifies intussusceptions, with findings similar to those found with CT. Magnetic resonance imaging reveals concentric bowel rings.
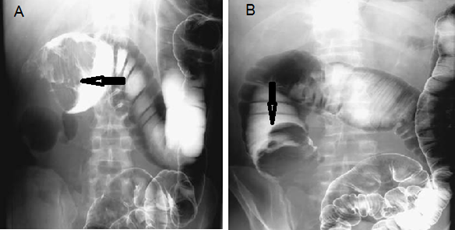
This is radiology images of colocolic intussusception with cecal carcinoma as lead point. A: Barium enema reveals the intussusceptum in the transverse colon (arrow). B: With further pressure the intussusceptum is reduced into the ascending colon.
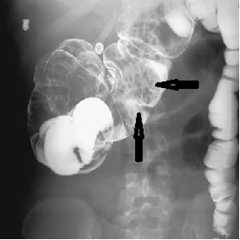
Radiology images of colocolic intussusception (arrows). The lead point was an endometrioma, a highly unusual source for an intussusception.
Pediatrics
An acute ileocolic intussusception in a young child is a common emergency. Most intussusceptions occur before the age of 2 years and are idiopathic in origin. The rare identifiable lead points, more common in older children, consist of a Meckel’s diverticulum, polyp, or even a duplication. Why the reported prevalence of intussusception is greater in some parts of the world is puzzling. The typical clinical presentation and conventional radiographic findings are well known. Occasionally encountered, however, is an atypical presentation, for instance, bilious vomiting due to an ileocolic mass resulting in extrinsic duodenal obstruction.
One variant is an ileoileocolic intussusception. Prereduction findings are similar to those of an ileocolic intussusception. Once the intussusception was reduced to the cecum, air enemas in nine children with ileoileocolic intussusceptions identified the intussusceptum as two or more separate polypoid components, in contrast to ileocolic intussusceptums, which tend to be either smoothly marginated or somewhat lobular in appearance. Sigmoidorectal intussusceptions also occur in infants and children. In some, the typical clinical presentation of a palpable abdominal mass and colicky pain is absent. These intussusceptions can be misdiagnosed as simple rectal prolapse.
Presumably a surgical consultation has been obtained and a surgeon has examined the child prior to attempted intussusception reduction. The child should be in stable condition, and both the surgeon and the radiologist should be confident that no contraindication exists to a therapeutic enema. Contraindications for reduction include bowel perforation, peritonitis, and hypovolemic shock. A long-term outcome study in children found an overall recurrence rate of 9%, with about two thirds of children having a single recurrence; reducibility was 95% for recurrent intussusceptions, with no perforations. Also, recurrence did not predict an abnormal lead point.
An acute ileocolic intussusception in a young child is a common emergency. Most intussusceptions occur before the age of 2 years and are idiopathic in origin. The rare identifiable lead points, more common in older children, consist of a Meckel’s diverticulum, polyp, or even a duplication. Why the reported prevalence of intussusception is greater in some parts of the world is puzzling. The typical clinical presentation and conventional radiographic findings are well known. Occasionally encountered, however, is an atypical presentation, for instance, bilious vomiting due to an ileocolic mass resulting in extrinsic duodenal obstruction.
One variant is an ileoileocolic intussusception. Prereduction findings are similar to those of an ileocolic intussusception. Once the intussusception was reduced to the cecum, air enemas in nine children with ileoileocolic intussusceptions identified the intussusceptum as two or more separate polypoid components, in contrast to ileocolic intussusceptums, which tend to be either smoothly marginated or somewhat lobular in appearance. Sigmoidorectal intussusceptions also occur in infants and children. In some, the typical clinical presentation of a palpable abdominal mass and colicky pain is absent. These intussusceptions can be misdiagnosed as simple rectal prolapse.
Presumably a surgical consultation has been obtained and a surgeon has examined the child prior to attempted intussusception reduction. The child should be in stable condition, and both the surgeon and the radiologist should be confident that no contraindication exists to a therapeutic enema. Contraindications for reduction include bowel perforation, peritonitis, and hypovolemic shock. A long-term outcome study in children found an overall recurrence rate of 9%, with about two thirds of children having a single recurrence; reducibility was 95% for recurrent intussusceptions, with no perforations. Also, recurrence did not predict an abnormal lead point.
Post a Comment for "Colocolic intussusception"