Management of portal hypertension
This depends on the cause and on whether the PV is still patent or not. The most pressing problem is likely to be bleeding from varices, especially oesophageal varices, and patients may present with melaena or haematemasis. Management may involve medical means, endoscopic techniques (either injection sclerotherapy of oesophageal varices or banding, in which a ring is placed around the base of the varix causing thrombosis), compression using a Sengstaken tube with an inflated balloon, surgical or percutaneous transjugular intrahepatic portosystemic shunt (TIPS). All these methods are relatively temporary, and can relieve pressure in the portal venous system, controlling portal hypertensive complications in order to plan further management.
TIPS is a percutaneous method used to relieve the symptoms of portal hypertension in cirrhotic patients. It connects the portal vein directly to the right hepatic vein with an expandable metal shunt A catheter and guide wire are passed, under X-ray control, through the jugular vein to the inferior vena cava (IVC) and into the hepatic vein. A pathway is then forged with a needle through the liver parenchyma to join the PV with the insertion of a shunt to keep the channel open. Portal venous blood then effectively bypasses the liver, flowing straight into the hepatic vein. This usually results in the speedy decompression of varices and improvement of other symptoms of portal hypertension.
Ultrasound may be used to monitor stent patency (Fig. below). Shunt stenosis or occlusion is a common problem, particularly in long-term shunts; this can be detected with routine postprocedure ultrasound screening and treated with reintervention. The most common site for a stenosis is at the junction of the stent with the PV. The velocity of blood flow in the shunt should be between 1 and 2 m/s and this should be consistent throughout the stent. A variety of Doppler parameters can be used to detect the malfunction of the shunt. A shunt velocity of less than 50 cm/s is a sign of stenosis but this has not been reproducible in all institutions, and other factors such as a change of 50 cm/s or more from the baseline scan, a localized elevation of velocity at the stenotic site (with an upper limit of normal of up to 220 cm/s) or an increase in the velocity gradient (as the stenotic stent exhibits an increased maximum velocity and a decreased minimum velocity) are also poor prognostic signs. TIPS is regarded as a temporary measure but can considerably improve the patient’s condition pending treatment of chronic liver disease, relieving haemorrhage from varices, relieving intractable ascites and stabilizing liver function. It is increasingly used as a bridge to liver transplant. It is also used as an alternative to surgery in patients who are poor surgical risks, although the diversion of blood away from the liver can result in adversely affected liver function and eventual encephalopathy.
TIPS is a percutaneous method used to relieve the symptoms of portal hypertension in cirrhotic patients. It connects the portal vein directly to the right hepatic vein with an expandable metal shunt A catheter and guide wire are passed, under X-ray control, through the jugular vein to the inferior vena cava (IVC) and into the hepatic vein. A pathway is then forged with a needle through the liver parenchyma to join the PV with the insertion of a shunt to keep the channel open. Portal venous blood then effectively bypasses the liver, flowing straight into the hepatic vein. This usually results in the speedy decompression of varices and improvement of other symptoms of portal hypertension.
Ultrasound may be used to monitor stent patency (Fig. below). Shunt stenosis or occlusion is a common problem, particularly in long-term shunts; this can be detected with routine postprocedure ultrasound screening and treated with reintervention. The most common site for a stenosis is at the junction of the stent with the PV. The velocity of blood flow in the shunt should be between 1 and 2 m/s and this should be consistent throughout the stent. A variety of Doppler parameters can be used to detect the malfunction of the shunt. A shunt velocity of less than 50 cm/s is a sign of stenosis but this has not been reproducible in all institutions, and other factors such as a change of 50 cm/s or more from the baseline scan, a localized elevation of velocity at the stenotic site (with an upper limit of normal of up to 220 cm/s) or an increase in the velocity gradient (as the stenotic stent exhibits an increased maximum velocity and a decreased minimum velocity) are also poor prognostic signs. TIPS is regarded as a temporary measure but can considerably improve the patient’s condition pending treatment of chronic liver disease, relieving haemorrhage from varices, relieving intractable ascites and stabilizing liver function. It is increasingly used as a bridge to liver transplant. It is also used as an alternative to surgery in patients who are poor surgical risks, although the diversion of blood away from the liver can result in adversely affected liver function and eventual encephalopathy.
the later stages. Vaccines exist for A and B, but not yet for the others. Hepatitis A and E are transmitted via contaminated food or drink and are particularly prevalent in third-world countries. Hepatitis B, C and D are likely to be transmitted through transfusion or sexual contact. Fulminant hepatitis, in which there is complete liver failure, is a rare complication of acute hepatitis B.Most patients with acute hepatitis recover completely, but hepatitis B, C and D may go on to develop chronic hepatitis. This has two forms:
● Chronic persistent hepatitis is a mild form of inflammation limited to the portal tracts. It is usually of comparatively little clinical significance and does not show ultrasound changes.
● Chronic active hepatitis is a more serious and aggressive form of the disease which causes diffuse, persistent inflammation. This may eventually lead to cirrhosis, which can be associated with HCC.
● Chronic active hepatitis is a more serious and aggressive form of the disease which causes diffuse, persistent inflammation. This may eventually lead to cirrhosis, which can be associated with HCC.
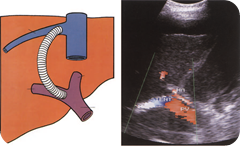
Ultrasound images of Transjugular intrahepatic portosystemic shunt (TIPS) & TIPS shunt in a patient with severe portal
hypertension. The higher-velocity MHA is seen anterior to the shunt, which demonstrates flow from right to left of the
image.
hypertension. The higher-velocity MHA is seen anterior to the shunt, which demonstrates flow from right to left of the
image.
Ultrasound images Thrombosed TIPS shunt. A
recanalized left portal vein (LPV) (arrow) can be seen
anterior to this.
but this has not been reproducible in all institutions, and other factors such as a change of 50 cm/s or more from the baseline scan, a localized elevation of velocity at the stenotic site (with an upper limit of normal of up to 220 cm/s) or an increase in the velocity gradient (as the stenotic stent exhibits an increased maximum velocity and a decreased minimum velocity) are also poor prognostic signs. TIPS is regarded as a temporary measure but can considerably improve the patient’s condition pending treatment of chronic liver disease, relieving haemorrhage from varices, relieving intractable ascites and stabilizing liver function. It is increasingly used as a bridge to liver transplant. It is also used as an alternative to surgery in patients who are poor surgical risks, although the diversion of blood away from the liver can result in adversely affected liver function and eventual encephalopathy.recanalized left portal vein (LPV) (arrow) can be seen
anterior to this.
LiveJournal Tags: Ultrasound images encephalopathy

I was diagnosed as HEPATITIS B carrier in 2013 with fibrosis of the
ReplyDeleteliver already present. I started on antiviral medications which
reduced the viral load initially. After a couple of years the virus
became resistant. I started on HEPATITIS B Herbal treatment from
ULTIMATE LIFE CLINIC (www.ultimatelifeclinic.com) in March, 2020. Their
treatment totally reversed the virus. I did another blood test after
the 6 months long treatment and tested negative to the virus. Amazing
treatment! This treatment is a breakthrough for all HBV carriers.